While the information contained in The Colonoscopy Chronicles will be as accurate as possible, it is not intended as medical advice. You should consult your personal physician regarding your own medical issues. So, you've had your colonoscopy, and now your doctor tells you that you have diverticulosis. You nod your head knowingly, since your doctor acts as if you should know exactly what that means, as she speeds on to her discussion about your hemorrhoids. But in reality, you really don't know what that means, and by now, it's too late to ask her. The recovery room nurse hands you a slick brochure telling you all about diverticulosis. You tell your friends at the health club the next day that they found diverticulosis, and suddenly your hearing stories about nuts, seeds, popcorn, Aunt Sally's ruptured colon, antibiotics, and now your head is swimming. After all, you just came her for a good workout and now your ready to check into the Mayo Clinic. Help!! Well-Doctor Mike is here to give you the Baby Boomer's Underground Guide to Diverticulosis. Stick with me, kid, you'll be fine! I am going to try and distill twenty three years of experience as a Gastroenterologist into a few paragraphs about diverticulosis-so please realize that this is not a comprehensive review of the topic. Rather, I am going to tell you the exact same thing that I tell my patients, what I consider the basics about diverticulosis.So here goes............ First of all,when the colonoscopy is over and we are reviewing the results, if diverticulosis is present, I let the patient know. I explain that it is a common finding-that probably at least 60-70% of people get diverticulosis. However, the good news is that the vast majority-perhaps 95% or so-will never experience any problems related to their diverticulosis. I go on to explain that diverticulae are little pouches in the colon,and while they are extremely common, we don't exactly know what causes them. There are many theories, most relating to the amount of dietary fiber we eat,but they are probably genetic to some extent, since they tend to run in families. I also explain that while the vast majority of people do not develop problems from the diverticulosis, the two major complications are diverticulitis, and bleeding. I explain that diverticulitis occurs when the pouches become infected. This leads to abdominal pain that is usually in the left lower part of the abdomen, and sometimes in the middle af the abdomen, below the navel. Other associated symptoms can include fever, or constipation. I advise patients to be aware of those type of symptoms and to seek medical attention right away if they occur, since they might need antibiotics to combat the diverticulitis. I explain that the bleeding associated with diverticulosis is usually painless, and sudden in onset. The bleeding is usually fairly severe when it occurs. Again, I advise patients to seek medical attention immediately if they have suspected diverticular bleeding. Finally, I explain to them that for years we advised patients to avoid nuts, seeds, and popcorn, on the theory that those particles are undigestible, and can get lodged in the diverticular pockets and cause diverticulitis. It seemed like a logical instruction-but the problem is, that it turned out that there was really no good evidence that ingesting nuts, seeds, and popcorn had anything to do with diverticulitis. Therefore, I currently do not restrict those items in my patients with diverticulosis, but rather just suggest a general high fiber diet. And that, my friends, is my "Readers Digest" version of diverticulosis. Naturally, this is a very simplified version of a very complicated topic. I did not touch on some of the less common, but very serious complications of diverticulitis, such as perforations, abscesses, or obstructions which may require surgical intervention. I also did not touch on those who have frequent, recurrent episodes of diverticulitis that may require elective surgery. But remember, these serious complications are not common. But because they may be fairly dramatic,even though they are not common, they get a lot of notoriety.
Wednesday, August 8, 2012
Thursday, July 12, 2012
Wednesday, July 4, 2012
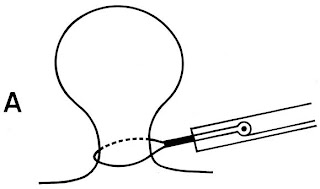
Removing Polyps With Snare
Snare Polypectomy We have discussed the use of the biopsy forceps to remove polyps. That technique is generally limited to the removal of smaller polyps-usually less than 5 millimeters. Larger polyps are generally removed using the snare technique. Just like the use of biopsy forceps, snares can be "hot" or "cold"-meaning that electrocautery is used or not used. A snare is basically a wire lasso that is placed around a polyp, then tightened around the polyp tissue to cut off the polyp.
Generally, the cold snare technique is limited to smaller polyps. The hot snare technique-ie the use of electrocautery-is employed in the removal of larger polyps since the cautery provides hemostasis(bleeding control) by essentially sealing off small blood vessels the may be severed during the removal of the polyp. Because polyps come in various shapes and sizes, the snare technique is adjusted based on the polyp. Let me give you an example. Some polyps are "pedunculated", meaning they grow on a stalk-almost like a cherry on a stem. To remove such a polyp, the snare is placed around the polyp, and the stalk is severed by tightening the snare and at the same time using electrocautery current through the wire. The diagram below shows a good representation of a snare polypectomy of a pedunculated polyp. Once the polyp has been removed with this technique, there is usually a small burn mark on the wall of the colon, as seen below(the small whitish area).
Posted by
Doctor Mike
at
8:35 PM
1 comments
![]()
Saturday, June 16, 2012
Polyp Removal Techniques The last post on this blog discussed some of the commonly encountered types of polyps. One of the goals of colonoscopy is to detect potentially pre-cancerous polyp-the distinct advantage of colonoscopy(versus imaging studies such as lower gi x-rays, or so called "virtual" colonoscopy is the ability to not only detect polyps, but to remove them at the same time. There are several techniques that are used by gastroenterologists. The choice of technique may depend on the size and shape of the polyp, as well as the experience, training, and comfort-level of the physician performing the procedure with the various techniques. I will try not to bore you technical details of each approach, but rather, I hope to give you a general idea of each so that if you or a loved one has a polyp removed you can have an idea of what exactly that meant. FORCEPS POLYPECTOMY Forceps are basically like a tiny set of tweezers. They are on the tip of a long wire-type device that we slide down the biopsy channel of the scope, and they emerge from an opening in the tip of the scope while it is in the colon. The assistant can open the forceps, then the physician positions the forceps over the polyp, then the assistanrt closes the forceps, thus grasping the polyp. The physician then basically just pluckes the polyp off the wall of the colon. Forceps can be "cold" or "hot". In the case of a cold forceps, there is no electric cautery involved, whereas in a hot forceps polypectomy, monopolar cautery is used. The advantage of cautery is that it can prevent bleeding, and can help destroy any redsidual polyp tissue on the colon wall that was not grasped with the forceps. The disadvantage is that sometimes the polyp tissue is destroyed by the cautery and difficult for the pathologist
Posted by
Doctor Mike
at
3:19 PM
0
comments
![]()
Friday, February 3, 2012
The Underground Guide to Polyp Removal!
How Are Polyps Removed?
We talked a little bit about colon polyps in our last post. Many patients are curious as to exactly how polyps are removed during colonoscopy. Today we will discuss that very topic. To be honest with you, the techniques we have for removing polyps during a colonoscopy are pretty amazing!
The vast majority of polyps are removed using:
1) Biopsy forceps- “cold” versus “hot”
2) Snare-“cold” versus “hot”
Biopsy forceps can be “cold” meaning that there is no electric current passing through the forceps, or they may be “hot” in which case monopolar electric current is transmitted to the tissue through the forceps. Polyps appropriate for removal with a biopsy forceps are usually quite small-up to 3 millimeters for a cold forceps and up to 4 mm for a hot forceps.
The forceps is really a tiny set of “tweezers” on a long wire that can be passed down a long hollow channel in the colonoscopy. The tweezers can be opened and closed by the technician assisting the colonoscopist. When a tiny polyp is identified, the forceps is slid down the scope, and the polyp is grasped with the open jaws of the tweezers which are then closed. If “hot” forceps are used, an electric current is passed through the forceps to obliterate the tissue, then the polyp is “plucked” off the wall of the colon with the forceps. The polyp tissue is then retrieved and sent to the pathology laboratory. If “cold” forceps are used, the polyp is grasped and plucked off the wall of the colon without any electric current.
Here is what a biopsy forceps looks like:
Here is the "business end" of a biopsy forceps:
Here is a polyp being removed with a "hot" biopsy forceps. Note the the polyp tissue is whitish color-the result of "blanching" of the tissue from the electric current:
Next time we will discuss the snare technique for polyp removal-so stay tuned!!
Posted by
Doctor Mike
at
2:11 PM
0
comments
![]()